Hi there, Michael Borozenets here, CTO at Fulcrum Rocks. We’ve been on quite an adventure with our latest project, Zuri Fertility. If you’re like us, passionate about making a difference in healthcare but find HIPAA compliance for software a bit of a head-scratcher, this article is for you.
Zuri Fertility wasn’t just another project for us; it was a commitment to ensure that we keep patient information safe and secure. We knew HIPAA compliance for software was crucial, not just because it’s a requirement, but because it’s the right thing to do. It was challenging, sure, but let me take you through our journey in a straightforward way, showing you how we tackled the complexities of HIPAA to bring Zuri to life.
This story is about more than just the technical bits. It’s about our dedication to protecting what’s private and making dreams come true for families. Join me as we dive into the essentials of making a healthcare app that’s not only effective but also respects and protects user privacy according to HIPAA standards. It’s simpler than you might think, and if we can do it, you can too.
Understanding HIPAA Requirements
HIPAA compliance for software revolves around the Privacy Rule, the Security Rule, and the Breach Notification Rule, each serving a pivotal role in safeguarding Protected Health Information (PHI).
For Zuri Fertility, compliance meant not only understanding these rules but implementing measures that reflect their essence in every facet of the application.
The Privacy Rule protects individuals’ medical records and other personal health information, the Security Rule sets standards for securing patient data stored or transferred electronically, and the Breach Notification Rule mandates the procedures for responding to data breaches.
Zuri’s Approach to HIPAA Compliance for Software
Zuri Fertility, through Fulcrum’s expertise, navigated the complex path to HIPAA compliance for software with strategic measures:
Conducting a Risk Analysis
A cornerstone of Zuri’s strategy was a comprehensive risk analysis aimed at pinpointing potential vulnerabilities within their Electronic Health Records (EHR) system. This proactive approach allowed the team to anticipate and mitigate risks, ensuring that PHI remained protected against unauthorized access or breaches.
Implementing Strong Access Controls
Adopting role-based access controls was a crucial step for Zuri. By defining specific roles within the EHR system, access to sensitive information was restricted solely to authorized personnel. This method not only complies with the HIPAA Security Rule but also minimizes the risk of internal data breaches.
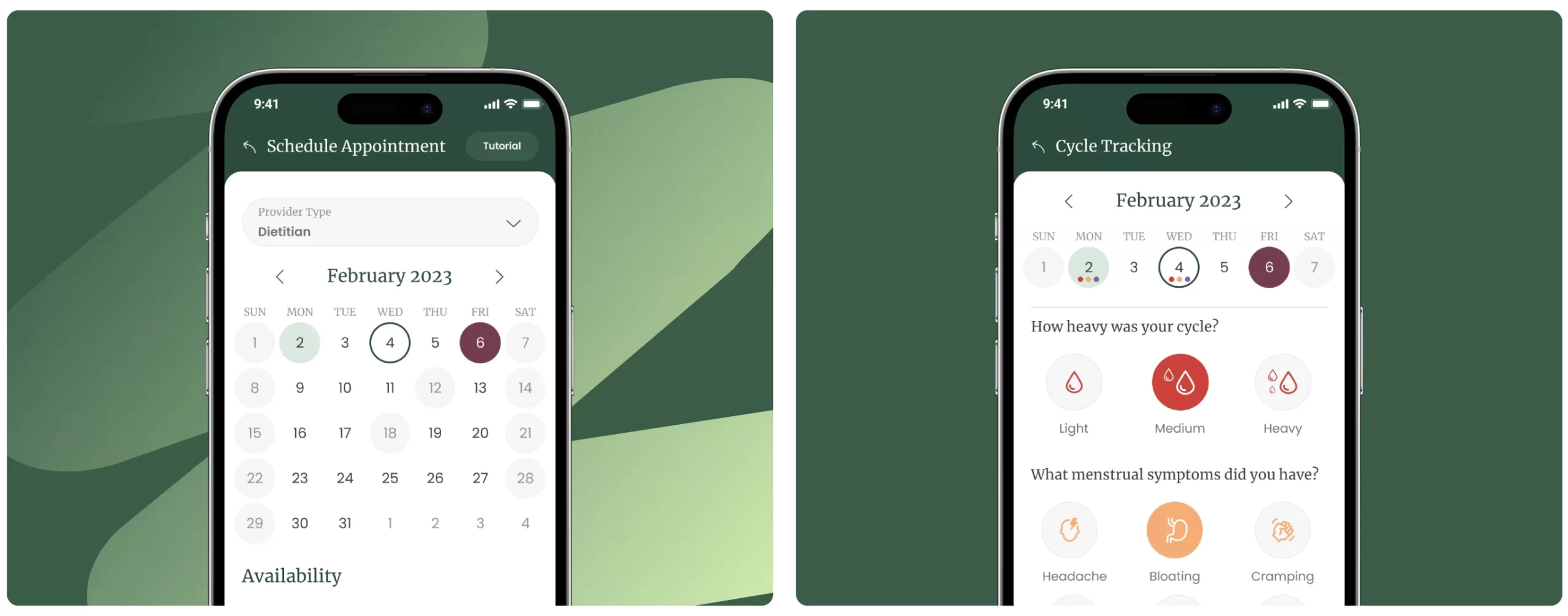
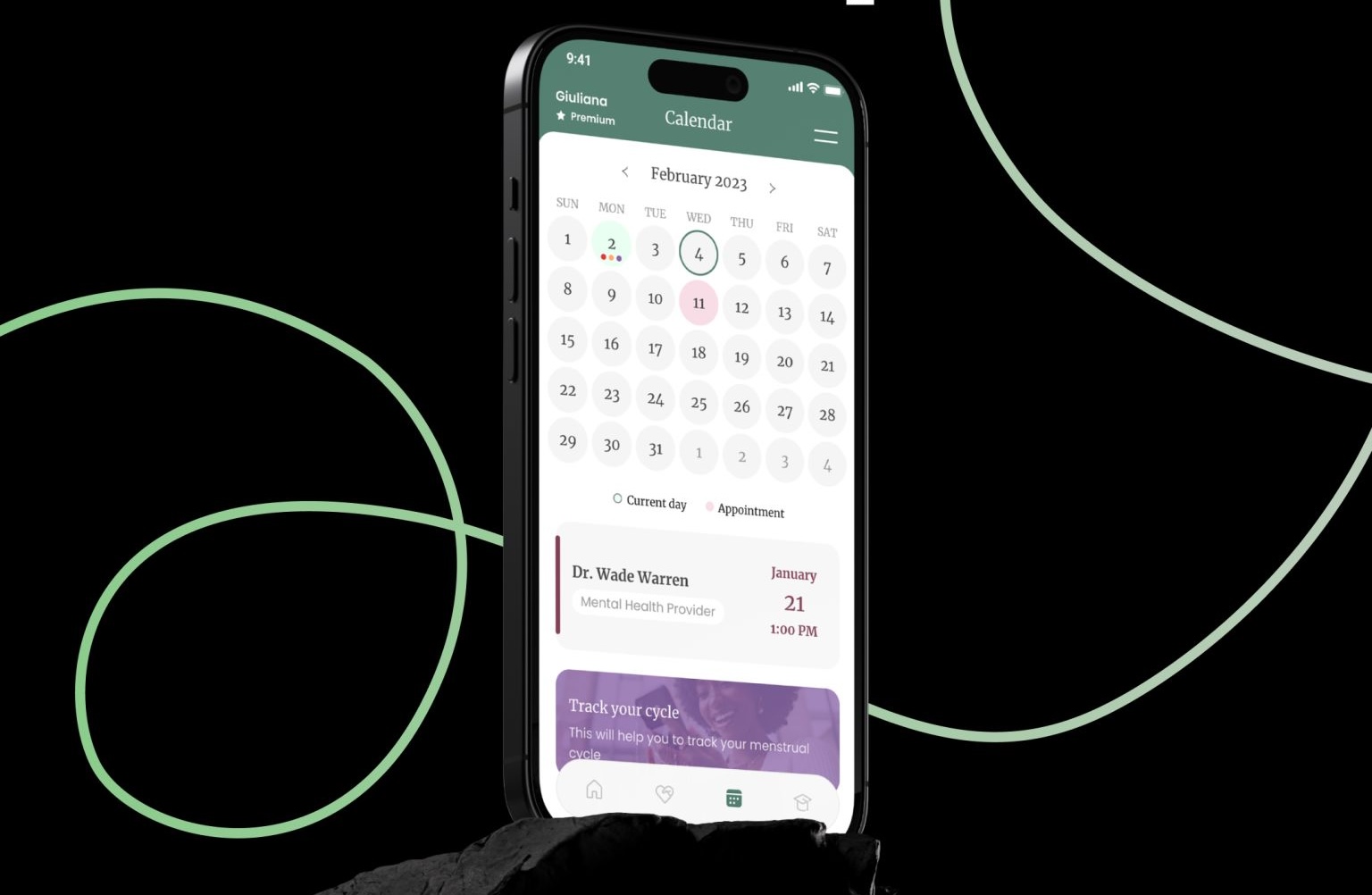
Enhancing Patient Rights
Zuri placed a strong emphasis on patient autonomy, revamping its patient portal to afford users effortless access to their health records. This initiative not only empowered patients but also aligned with the HIPAA Privacy Rule’s provisions on patient rights, including record amendments and disclosures.
Training Employees
Aware of the potential for human error, Zuri instituted a rigorous training program for all employees. This program emphasized the significance of PHI, the essentials of HIPAA compliance, and the specific protocols established by Zuri to prevent data mishandling.
Establishing a Breach Notification Protocol
Zuri prepared for the possibility of data breaches by setting up a robust breach notification protocol. This included prompt investigation procedures, timely notification to affected individuals, and strategic measures to avert future incidents, all in compliance with the Breach Notification Rule.
Challenges and Solutions
Zuri faced several challenges, such as integrating HIPAA compliance into its existing workflows and ensuring continuous employee training. Solutions included adopting a phased approach to compliance and utilizing technology to streamline and automate compliance-related tasks.
What’s next?
Wrapping up our story with Zuri Fertility, it’s been quite the ride. Through all the tech lingo, the coding marathons, and the endless cups of coffee, the biggest takeaway is pretty simple: it’s all about keeping trust at the core of everything we do. HIPAA might seem like just another set of rules, but for us, it was a roadmap to earning that trust, every step of the way. You can learn more about our Healthcare software development services here.
Our journey wasn’t just about ticking boxes or meeting standards. It was about ensuring that when someone trusts us with their dreams, we protect those dreams like they’re our own. As we move forward, Zuri Fertility stands as a beacon for anyone stepping into the digital health space. Yes, it’s about building something great, but it’s also about building it right—secure, trusted, and patient-centered.
Before I sign off, I want to leave you with something practical: a HIPAA compliance checklist. We know firsthand that the journey to compliance can feel like navigating a maze without a map. This checklist is here to help.
However, given the complexity and nuances of HIPAA regulations, it’s advisable to consult with legal experts specializing in healthcare law to ensure comprehensive compliance strategies tailored to your specific operations.
HIPAA Compliance for Software - Checklist for Healthcare Startups
-
Understand HIPAA RulesFamiliarize yourself with the HIPAA Privacy, Security, and Breach Notification Rules. Knowing these rules is the first step to ensuring compliance.
-
Identify Protected Health Information (PHI)Understand what constitutes PHI and ePHI (electronic PHI) within your organization. Make sure all team members know the types of information that must be protected.
-
Conduct a Risk AnalysisRegularly perform a comprehensive risk analysis to identify potential vulnerabilities to the confidentiality, integrity, and availability of ePHI. This analysis is crucial for setting up proper security measures.
-
Develop and Implement Policies and ProceduresBased on the risk analysis, develop and implement security policies and procedures designed to protect PHI and ensure HIPAA compliance. These should be documented and accessible.
-
Train EmployeesConduct regular training sessions for all employees handling PHI, ensuring they understand the organization's policies and procedures, as well as their individual roles in protecting patient data.
-
Secure Patient DataImplement physical, administrative, and technical safeguards to protect PHI. This includes encryption, secure access controls, and network security measures.
-
Manage Vendors with Access to PHIEnsure that all business associates and vendors who have access to PHI are also compliant with HIPAA regulations. This typically involves executing business associate agreements (BAAs).
-
Establish a Patient Rights PolicyDevelop policies that allow patients to access their health records, request amendments, and receive an accounting of disclosures, in accordance with the HIPAA Privacy Rule.
-
Report Breaches PromptlySet up a protocol for identifying, reporting, and responding to any PHI breaches. The Breach Notification Rule requires covered entities to notify affected individuals, HHS, and, in some cases, the media, within specific time frames.
-
Regularly Review and Update Compliance EffortsHIPAA compliance is not a one-time effort. Regularly review and update your risk management strategies, policies, and training programs to adapt to changes in regulations, technology, and your own operations.
-
Document EverythingMaintain thorough documentation of all HIPAA compliance efforts, including risk analyses, policies, training sessions, and breach response efforts. This documentation is essential for demonstrating compliance during audits or investigations.
What happens if there’s a breach?
In 2015, Anthem, Inc., one of America’s largest health insurers, experienced a cyberattack that led to the largest health data breach in history, compromising the personal information of nearly 79 million individuals. This incident spotlighted the dire consequences of failing to adequately protect sensitive patient data. As a result, Anthem agreed to pay a record $16 million to the U.S. Department of Health and Human Services Office for Civil Rights (OCR) to settle potential HIPAA Privacy and Security Rules violations. This settlement is the largest in the history of HIPAA enforcement actions, underscoring the critical need for robust security measures and compliance strategies.
The Cost of Non-Compliance
The financial impact of healthcare data breaches has been rising, with the average cost reaching about $7.13 million in 2020, marking it as the highest across any industry for the tenth consecutive year (The National Law Review).