Shortly speaking, the difference between HL7 vs FHIR can be roughly summarized with this image below:
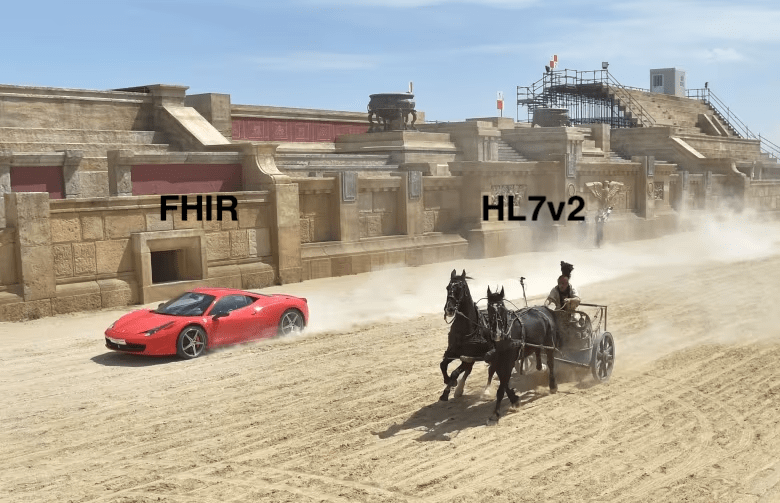
Only, it’s not that simple, as HL7v2 still has highest adoption rate, which means going with FHIR might be complicated. Let’s explore.
When should you worry about interopeability?
FHIR and HL7v2 differences come onto stage whenever you need to ensure interoperability on the following scenarios:
- You need to connect to EHR. Using HL7 & FHIR might help to achieve seamless communication and data exchange between electronic health record (EHR) systems and other healthcare apps
- You need to exchange clinical data such as lab results, imaging studies, and medication orders, between healthcare providers and systems.
- You might want to enable patients to share data with healthcare providers and applications.
- Collect and analyze healthcare data from multiple sources to identify trends, manage chronic conditions, and improve population health outcomes.
Whatever the reason, different versions of HL7 have unique features, benefits, and difficulties. Choosing the right version depends on factors like project needs, interoperability requirements, and existing systems. It’s crucial to know the distinctions between HL7 standards and consider things like compatibility, complexity, and industry trends when picking the best version for a healthcare integration project.
What’s FHIR Standard?
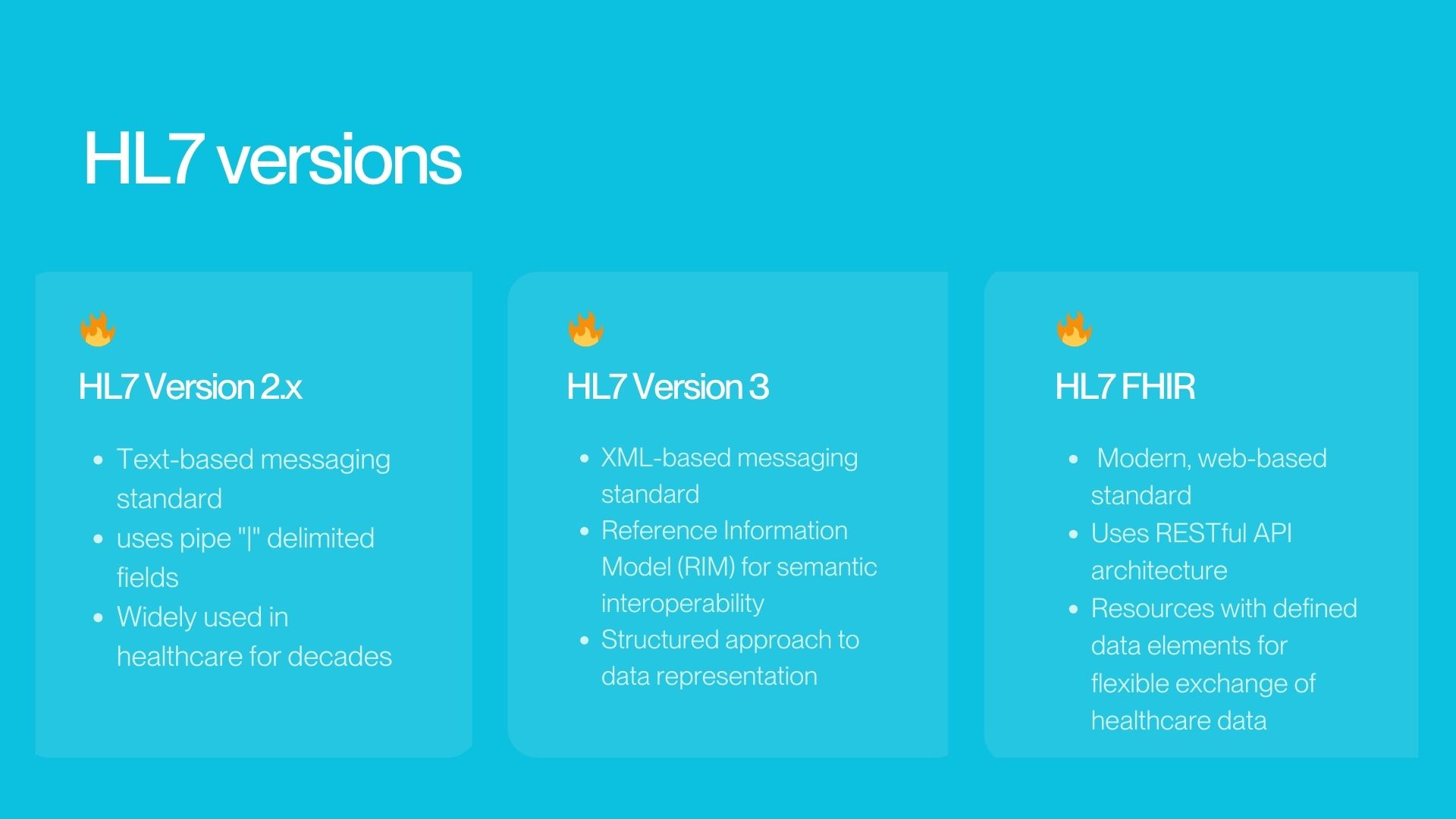
HL7 FHIR stands for Fast Healthcare Interoperability Resources. It is a modern, web-based standard for healthcare data exchange, making it simpler than older HL7 standards. It uses a modern method called RESTful API and defined data elements, making data exchange easier and more flexible. FHIR standard is becoming popular in healthcare because it’s simple, adaptable, and supports modern web technology.
What is HL7v2 in Healthcare?
HL7v2, or Health Level Seven version 2, is a widely used standard for exchanging healthcare information electronically. It’s framework used by majority of healthcare organizations to structure messages containing clinical, admin and other Healthcare data. HL7v2 messages typically use text-based formats and follow a defined structure. FHIR mentioned above is the latest HL7 version.
Is HL7v2 outdated?
Well, the HL7v2 standard was introduced in 1989, which is way before Internet, iPhones and modern interfaces. It’s been successful, and it did it job well. But, obviously, it has significant limitations:
- Doesn’t supper modern technologies. HL7v2 wasn’t made for newer web-based tools and ways of sharing information. This means it doesn’t work well with modern tech like web APIs, which many systems use now. That’s why it’s tough to share information smoothly and slows down making new healthcare tech.
- Doesn’t handle images or static documents. HL7v2 messages can’t show complex healthcare data well because they’re mostly text-based. This makes it hard to share detailed health information like test results or X-rays in a way that all systems understand.
- Software Engineers need much more time to learn how to work with HL7v2.
- Lack of Semantics: HL7v2 messages don’t always have clear meanings for data. This means that different systems might see the same information differently, which can lead to mistakes in how doctors make decisions.
- It’s reached its ceiling in terms of innovation and improvement.
In this case, why HL7v2 is still so widespread?
- In the United States, almost 95% healthcare organizations use HL7v2 interface rules.
- Also, over 35 countries worldwide have adopted HL7 interfaces.
Moving from HL7v2 is not easy, as there are certain limitations to how FHIR systems connect to HL7 systems. We will talk about that later.
What’s more, depending on what product you seek to build you might need to actually stick with HL7v2 . It depends on healthcare systems your product needs to integrate with.
Is FHIR standard superior to HL7v2?
What makes FHIR easier to use and understand is its simple and flexible design. Here are a few reasons why:
Clear Rules: FHIR follows clear and consistent rules for organizing and sharing health information. It’s like having a playbook that everyone can follow, making it easier to understand how things work.
Standardized Format: FHIR uses standard formats like JSON and XML, which are widely used and understood by developers. It’s like speaking a common language that everyone knows, so there’s less confusion.
Modular Approach: FHIR breaks down health information into small, easy-to-understand pieces called “resources.” Each resource represents a specific type of data, like a patient or a medication. It’s like having building blocks that you can put together in different ways to create whatever you need.
Flexible Structure: FHIR allows for customization and extension to fit different needs. It’s like having a toolbox with tools that you can use to build exactly what you want, without being limited by rigid rules.
Community Support: FHIR has a large and active community of developers and healthcare professionals who contribute to its development and improvement. It’s like having a team of people working together to make things better and easier for everyone.
Overall, FHIR’s simplicity, standardization, modularity, flexibility, and community support make it easier for developers and healthcare providers to understand and use effectively. It’s like having a user-friendly toolkit for sharing health information in a more streamlined and efficient way
Can FHIR Connect to systems supporting HL7v2?
Let’s say you decided to go with FHIR. Would there be issues with connecting to HL7v2? Well, short answer: there’re might be. Connecting FHIR with older HL7v2 systems might need extra work, like using translation software.
- The extent to which you can connect with a legacy system using FHIR depends on how much that system supports FHIR.
- Direct support for FHIR makes connecting easier and allows for real-time data exchange.
- Conversion tools can help connect FHIR with systems that don’t support it directly, but they might add complexity.
- While FHIR aims to cover all healthcare information exchange, there may still be some cases where older HL7 standards offer more detailed solutions.
How do I use FHIR when connecting to EHRs?
Many major EHR vendors and healthcare IT companies have announced support for FHIR and are actively incorporating FHIR interfaces and APIs into their products. What’s more, government regulations such as CMS (Centers for Medicare & Medicaid Services) Interoperability and Patient Access final rule in the United States have encouraged adoption of FHIR.
Therefore, if you wish to connect to EHRs, using FHIR, here’s what to do:
- Check for FHIR Support: First, see if the EHR system you want to connect to supports FHIR. Many EHR systems now work with FHIR to let outside apps access patient data.
- Use FHIR APIs: If the EHR system supports FHIR, use FHIR APIs to talk to it. FHIR APIs help you get patient data, add new info, update records, and do other things using standard internet methods.
- Leverage FHIR Resources: FHIR has standardized resources for different types of healthcare data, like patients, medications, and observations. When connecting to an EHR system with FHIR, you’ll use these resources to exchange patient info.
- Implement FHIR Integration: Set up your app to talk to the EHR system using FHIR. This might involve building FHIR-friendly features, using FHIR tools in your software, and dealing with FHIR data formats.
- Handle Authentication and Authorization: Make sure your app follows security rules for getting patient data from the EHR system. This could mean using special ways to log in and making sure you’re allowed to access patient records.
- Test and Validate: Before using your app for real, test it well with the EHR system. Check that it can exchange data like it should and that patient info is correct.
How to use FHIR when sharing clinical data?
In case you need to share clinical data of various complexity, here’s what you need to consider, when you choose between FHIR vs HL7v2.
- Evaluate how detailed and complex your clinical data is. FHIR handles complex data better than HL7v2.
- Check if your current systems work well with FHIR or HL7v2. Some may support one better than the other.
- Think about how well each standard will grow with your organization’s needs. FHIR is more modern and flexible for future changes.
- Regulations: Make sure you follow any rules or laws about data exchange. Some regulations may require using FHIR.
- Vendor Support: Check if your EHR vendor and other partners support FHIR or HL7v2. It’s easier if your vendors already work with the standard you choose.
By taking all of the above into account, you can decide whether FHIR or HL7v2 is best for your clinical data exchange needs.
| HL7 Version 2.X | HL7 FHIR | |
|---|---|---|
| Interoperability | Limited interoperability due to variations in message structures and semantics between systems. | Designed for enhanced interoperability with a focus on simplicity, modularization, and web-friendly RESTful APIs. It facilitates easier integration and data exchange between systems. |
| Development Approach | Evolves through incremental updates and extensions but lacks a unified approach to data modeling and messaging. | continuous updates, modularization, and extensibility |
| Implementation Complexity | Relatively straightforward to implement but lacks standardization in message structures and vocabulary. | It's modular design and RESTful APIs simplify integration and development efforts. |
| Adoption & Community | Widely adopted in the healthcare industry but faces challenges in semantic interoperability and extensibility. | rapid adoption and community support due to its modern design, clear documentation, and active engagement with developers |
Checklist for choosing FHIR or HL7v2
-
What type of clinical data do we need to exchange?If you have a good understanding of how complex your data should be, you will see what standard is better for you.
-
What are the interoperability requirements of our organization?Assess interoperability needs, including data exchange frequency, partner systems, and regulatory compliance.
-
Are our current systems compatible with FHIR or HL7v2?If you evaluate compatibility of current systems, it will let you determine ease of implementation.
-
How scalable do we need our clinical data exchange solution to be?
-
What are the regulatory and compliance requirements for clinical data exchange?
-
What level of support and adoption does each standard have within the industry?Investigate the level of support and adoption by EHR vendors, healthcare IT companies, and industry stakeholders can provide insights into the feasibility and alignment of each standard with industry best practices.
-
How do FHIR and HL7v2 compare in terms of features, flexibility, and ease of implementation?You can learn all of this in this very article.
Why as a founder you need to understand differences between FHIR & HL7?
Obviously, if your startup’s product needs to connect with existing healthcare IT systems, knowing HL7 standards is really important. What’s more, several healthcare rules, like HIPAA in the U.S., demand standard formats for sharing electronic health data. HL7 standards are often necessary to meet these rules.
As a healthcare startup founder, you should have a basic understanding of HL7 standards, especially in these scenarios:
- If your startup gathers data from various places like EHR systems, labs, imaging, and wearables, HL7 standards can help blend and handle this data effectively.
- HL7 standards are key in health information exchange initiatives, where organizations share patient data across boundaries. If your startup works on solutions for this or joins HIE networks, HL7 expertise is crucial.
- If your startup intends to collaborate with other healthcare groups or link with third-party systems, HL7 compatibility might be necessary.
How to oversee a project involving HL7 integration if you are non-technical?
-
Test and validateCheck that the integrated systems share healthcare info correctly. Test different situations to see if HL7 messages are understood and sent right.
-
Evaluate system speedKeep an eye on how fast the systems exchange data. Assess factors like response time, system reliability, and scalability.
-
Get feedback from doctors & labsGet feedback from doctors or users of your product. Their input will highlight any usability issues.
-
Problems ResolutionSee how quickly your team solves any issues that come up. Make sure they can figure out and fix technical problems fast.
-
Check documentationClear and comprehensive documentation indicates that your developers have thoroughly documented their work.
What are the risks of wrong HL7 vs FHIR implementation?
It’s worth it to make sure that HL7 is implemented correctly. Here’s why:
- Wrong Data: Healthcare data might be inaccurate, leading to wrong diagnoses or treatments, risking patient safety.
- Communication Issues: Systems may not exchange data well, causing breakdowns and inefficiencies in healthcare delivery.
- Breaking Rules: Not following healthcare regulations like HIPAA could result in legal penalties.
- Workflow Problems: Delays in patient care or administrative errors could disrupt healthcare workflows.
- Higher Costs: Fixing errors can be expensive and time-consuming, increasing project costs.
In summary, incorrect HL7 integration could lead to serious problems like patient safety risks, legal issues, workflow disruptions, and damage to your organization’s reputation. It’s crucial to get HL7 integration right to avoid these risks.
Need help with implementing FHIR vs HL7?
At Fulcrum we are focused on Healthcare businesses and organizations, it’s our bread and butter. If you need help moving from Hl7 to FHIR or related requests, give us a call. Read about Healthcare software development services here on this page.